Friday, December 28, 2007
ADA Revises Nutrition Recommendation for those with Diabetes
While I finish reading the actual documents and write up what I think of the paper, here are links to what others are saying today:
Jimmy Moore - New 2008 ADA Recommendations Partially Acknowledge Low-Carb Diets
Adam Campbell - Apparently Hell Just Froze Over
Dr. Mary Vernon - HAS THE AMERICAN DIABETES ASSOCIATION SPARKED YET ANOTHER ATKINS REVOLUTION?
Sunday, December 23, 2007
Friday, December 21, 2007
What If Saturated Fat Is Not the Problem?
Here’s an idea to chew on: The carbs in your diet tell your body what to do with the fat you eat, so it’s the type and amount of carbohydrates that matter when it comes to your weight and health.
Virtually every bit of health information today includes the advice to avoid saturated fat — the so-called evil stuff that lurks in animal foods like steak and eggs. The basis for this recommendation is that research has shown a correlation between saturated fat intake and total cholesterol and LDL (“bad cholesterol”). The problem with these studies is that the effects are not large, there is wide variation among individuals and, in most of these studies, the predicted benefit in incidence of cardiovascular disease did not materialize. In addition, we now know much more about risk factors for cardiovascular disease (CVD) beyond LDL. No assessment of CVD risk can be made without considering HDL (“good cholesterol”), triglycerides, and the size of the LDL particle. Plenty of research shows that these markers can worsen when people reduce their intake of saturated fat and that they can improve by reducing the intake of carbohydrates.
You don’t have to be a medical researcher to recognize that this is a politically charged issue. The thing that is missing for the public is an impartial evaluation of all the data on saturated fat. My personal opinion is that there is much contradictory data and a recent review of the situation suggests that there is not sufficient evidence to make any recommendations.
There is a sense that, in the absence of definitive evidence, lowering saturated fat will at least do no harm. This is not right. The problem for people with diabetes is what happens when saturated fat is replaced with carbohydrate, and research has repeatedly shown that this may actually be harmful. Consider that, according to the Centers for Disease Control and Prevention, during the onset of the current epidemic of obesity and diabetes, almost all of the increase in calories in the American diet has been due to carbohydrate. The percent of total fat and saturated fat in our diet decreased. In men, the absolute amount of saturated fat consumed decreased by 14 percent!
One of the most striking reasons to doubt the across-the-board proscriptions against saturated fat is the report from the large scale Framingham study in the Journal of the American Medical Association, titled “Inverse association of dietary fat with development of ischemic stroke in men.” You read that right: The more saturated fat in the diet, the lower the incidence of stroke.
Perhaps the most compelling research was published in a 2004 issue of the American Journal of Clinical Nutrition by researchers from the Harvard School of Public Health. Their study showed that, in postmenopausal women with heart disease, a higher saturated fat intake was associated with less narrowing of the coronary artery and a reduced progression of disease. Even with similar levels of LDL cholesterol, women with lower saturated fat intake had much higher rates of disease progression. Higher saturated fat intake was also associated with higher HDL (the “good” cholesterol) and lower triglycerides.
If saturated fat isn’t the problem, what is?
In this study, in which greater saturated fat intake was associated with less progression of coronary atherosclerosis, carbohydrate intake was associated with a greater progression. Carbohydrate, through its effect on insulin, is the key player. Insulin not only sweeps up glucose from the blood but it also plays air traffic controller, making the call as to whether that glucose is turned into fat or is used for energy. Most importantly, insulin determines what happens to dietary fat — whether it gets stored or oxidized for fuel. In fact, the fat profile in the blood (cholesterol and triglycerides) is not strongly tied to diet.
A recent study by Jeff Volek at the University of Connecticut compared low-carbohydrate and low-fat diets. Even though the low-carbohydrate diet had three times as much saturated fat as the low-fat diet, levels of unhealthy fats in the blood were lower in the low-carbohydrate group. How is that possible? That is what metabolism does.
What is the best diet?
We don’t know the ideal diet composition. We do know that saturated fat, unlike trans-fat, is a normal part of body chemistry and extreme avoidance is not justified by current scientific data. Removing some saturated fat to reduce calories is good, but adding back carbs appears to be deleterious. It appears that healthy, carbohydrate restriction will trump the effects of any kind of fat. For a person with diabetes, blood glucose must be the first consideration. If you have relatively tight blood sugar control, the amount of saturated fat you eat may be a non-issue. You can do what we did before the diabetes-obesity epidemic: regulate your intake by your taste and your natural appetite. No one ever did want to eat a pound of bacon.
Sources:
1. Food and Nutrition Board: Macronutrients. In: Dietary reference intake: National Academies Press; 2005, p.484.
2. JB German, CJ Dillard: Saturated fats: what dietary intake? Am J Clin Nutr 2004, 80:550-559.
3. MW Gillman, et al. : Inverse association of dietary fat with development of ischemic stroke in men. JAMA 1997, 278:2145-150.
4. D Mozaffarian, EB Rimm, DM Herrington: Dietary fats, carbohydrate, and progression of coronary atherosclerosis in postmenopausal women. Am J Clin Nutr 2004, 80:1175-1184.
5. JS Volek, et al. A hypocaloric, very low carbohydrate, ketogenic diet results in a greater reduction in the percent and absolute amount of plasma triglyceride saturated fatty acids compared to a low fat diet. NAASO, Boston, MA, October, 2006.
Thursday, December 20, 2007
Obesity: Is it a Form of Malnutrition?
"Even a brief visit to Czechoslovakia would reveal that obesity is extremely common and that, as in other industrial countries, it is probably the most widespread form of malnutrition."
This idea, the obesity is a form of malnutrition, isn't new and there is increasing data pointing to nutrient deficiency as contrbuting to the growing prevalance of overweight and obesity around the world.
How can that be though? Don't a number of studies point to our increasing calorie intake, along with a more sedentary lifestyle, as the cause of our growing waistlines?
While it is difficult to believe that one could be deficient for essential nutrients - vitamins, minerals, trace elements, essential fatty acids, and essential amino acids - while consuming so much food, let's see what the published data tells us.
Back in Janaury I wrote about a study out of Sweden that found four-year-old children already insulin resistant and overweight. One statistically significant finding was that the heaviest children were those consuming the least amount of dietary fat; they were also found to be deficient in vitamin D, iron and omega-3 fatty acids. Yet they were classified as obese. How did they manage to eat too much yet fail to meet nutrient intake levels for health and well-being?
In 2000 a survey of workers at a fertilizer plant revealed that many were overweight and obese - concurrent with their intake of excess calories they were found to be deficient in vitamin A, thiamin (B1) and consumed a poor ratio of mineral salts. The researchers concluded "Hyper-energetic, disbalanced nutrition, and incorrect nutritional-behavioral model are factors that determine the prevalence of overweight and obesity among the workers examined."
A study published last summer concluded that "Vitamin D insufficiency was associated with increased age, BMI, and SBP, and decreased HDL-C."
Just this month, a stunning paper was published examining the presence of micronutriet deficiencies in women. The researcher, Dr. Aswaf "examine[d] the relationship between micronutrient deficiency and the prevalence of mothers' overweight/obesity in Egypt using the 1997 Egyptian Integrated Household Survey. The ordered logit results show an overlap between micronutrient deficiency and the prevalence of mothers' overweight/obesity in Egypt. The odds of being overweight/obese are 80.8% higher for micronutrient deficient mothers than for non-deficient mothers, keeping all other variables constant."
Lastly, and by no means the end of the data we could look at, data published from the NHANES surveys tell us something really interesting - over the last few decades our intake of protein has remained stable, level, not increased; our intake of fats and oils has also remained stable; our intake of carbohydrate has increased - yet deficiency in critical nutrients is increasing amongst the population, with too many Americans failing to meet requirements for Vitamin E, C, A and D, selenium, magnesium and potassium.
With just these few studies, there appears to be a connection between micronutrient intake and excess weight - malnutrition parallel to an overweight or obese body state.
For some time now, I've written about how the dietary recommendations are flawed. They're focused on macronutrient ratios - carbohydrate, protein and fat - with the assumption being that if you follow such an eating pattern, you'll meet micronutrient requirements.
One small problem - even the menus published by the government and medical organizations to provide an example to the public of how to eat are nutritionally deficient for critical essential micronutrients. In fact, I've even posted side-by-side menus that showed the recommended diet compared to a controlled-carb diet was nutritionally inferior to the controlled-carb menu. In such comparisons, I use menus that are published by organizations rather than create them myself to reduce any chance for bias on my part.
So, I wasn't surprised to learn about a new study that Cassandra Forsythe wrote about a couple of weeks ago.
Go ahead - go take a peek - it's worth the read!
Wednesday, December 19, 2007
Growing Pains
Its recommendations should make any parent shudder - not only does the position of the AAP assume overweight and obesity in children is a problem of behavior, it assumes every child in the United States, with the exception of those classified as "underweight" by BMI, is in need of routine intervention and prevention to avoid overweight and obesity in adulthood.
I kid you not.
Every child in the United States, except those with a BMI classifed as "underweight," will now be subject to a risk assessment and prevention measures at every doctor visit. The implication within the document is clear - parents simply cannot be trusted to know how to raise normal healthy weight children over the long-term, even when their child is a normal weight, thus routine, repeated messages must be delivered at each and every opportunity.
The new guidelines call for healthcare professionals to question and investigate all of your family behaviors and habits at home - everything from what you eat, when you eat, how often you watch television or use a computer, if you eat out, where and how often, and how much time is spent being sedentary versus being active is to be collected and noted in your childs medical chart.
Despite the fact your child is classified within a "healthy weight" you'll be subject to your own scrutiny as a parent too - if you're overweight or obese, your child will be flagged as "at risk" due to your weight, not their weight.
Should the clinician note any abberant behavior - heaven forbid you allow your child, for example, a level of television time deemed excessive - you'll be scolded to limit television time. Heck, even if nothing is found and all is well, you'll still get the lecture about diet, exercise, limiting fast food and avoid sugary drinks....just in case....overweight and obesity is, afterall, a problem of behavior and you need constant reminder of that if you are to comply.
Where the guidelines sink to Brave New World levels is what is recommended for those children who have a BMI classed at or above the 85th percentile. There is to be no more sugar-coating the problem. Children with a BMI between the 85th and 94th percentile are overweight and children at or above the 95th percentile are obese.
In addition to the above assessments of risk, they'll now be subject to routine bloodwork and you'll be expected to do something about the "problem behaviors" now.
The first stage will be "Prevention Plus" through your doctors office. You'll now be expected to visit the doctors office for monitoring more frequently and ensure your child eats 5+ servings of fruits and vegetables daily, ideally eliminate sweetened beverages from your child's diet or limit to 1 per day, limit television time to less than 2-hours per day, make your child do physicial activity for 1+ hours per day, prepare meals at home, eat at the family table 5-6 times per week, have a "healthy" breakfast daily, and get the whole family on-board with the changes. You'll have 3-to-6 months for the doctor's office to see results, with visits scheduled to follow-up and monitor each month, and if no progress is noted, you and your child will be bumped to stage 2.
Stage 2 assumes you didn't do enough on your own, so now you and your family will be expected to follow a "structured" planned menu, reduce television time to less than 1 hour per day, engage in planned "supervised" physical activities and record what you are doing to prove you're complying with the recommendations and "achieving targeted behaviors"! If progress is not noted within three to six months, yup, you'll be bumped to stage 3.
In stage 3 you'll enjoy an intervention team (note sarcasm) that includes a behavior counselor (social worker, physcologist or other mental health provider), registered dietitian, exercise specialist and primary care provider, as well as weekly office visits to monitor progress in the "structured program in behavior modification" which will include, "at minimum", food monitoring, short-term diet and physical activity goal setting and "contingency management."
This "Comprehensive Multidisciplinary Intervention" now intensifies the urgency and seeks to maximize "behavior changes." That's because, if all this fails to result in progress and a reduction of BMI to the "healthy weight" category, they're going to pull out the big guns and take your child to stage 4 - the "Tertiary Care Intervention," which can include admission to a tertiary care facility for children as young as two, very low-calorie diets for children as yound as two, medications for children as yound as six, and/or bariatric surgery for children older than twelve.
Within the link above is the second document, Assessment of Childhood and Adolescent Overweight and Obesity, which details how to determine if a child is overweight or obese and reinforces the need for intervention, even in healthy, normal weight children. Noteworthy in this document is the explicit determination that BMI is the end-all-be-all measure of risk. While they note the BMI has flaws, and that the use of calipers to determine fatness is useful - "skinfold thicknesses are predictive of body fat in children and adolescents" - they continue on to dismiss its use and state "the expert committee does not recommend the routine clinical use of skinfold thickness measurements in teh assessment of childhood obesity."
What this means is that if you have an athletic, muscular child, who happens to have a high BMI due to muscle, you're going to be expected to do something about his/her weight to bring BMI to a "normal healthy" range.
Throughout the document the expert committee goes to great lengths to detail how to ask questions of parents and children, what to look for as problematic behaviors, and how to convince parents to modify those problematic behaviors.
A third document within the PDF package, Recommendations for Prevention of Childhood Obesity, we learn the justicification of the new guidelines in the opening sentences, "The majority of US youth are of healthy weight, but hte majority of US adults are overweight or obese. Therefore, a major health cahllenge for most American chidlren and adolescents is obesity prevention - today, and as they age into adulthood."
Let's not address what caused adults in this country to grow heavier, let's just continue to assume it's gluttony and sloth, lack of willpower, eating too damn much food, being lazy and more - those bad, bad, bad behaviors - and not allow our children to fall into the same trap and repeat, repeat, repeat to children they must eat a healthy diet and exercise daily!
We must do this, even if they're a healthy weight now, because - by golly - look at the adults around them! Bad examples, bad behaviors, bad, bad, bad.
Within the document we find lots of suggestions about how to monitor, control and modify behaviors - everything from positive reinforcement to cognitive restructuring to self-assessment to decision support.
Then there is the Recommendations for Treatment of Child and Adolescent Overweight and Obesity document. In it we're treated to the dogma to eat a "healthful" diet before getting to the real meat of the purpose - sections on food behaviors and then dietary intervention that includes the "use of balanced macronutrient/low-energy diets" for our children as a means to an end.
This is followed with reminding readers about the importance of physical exercise and the role of structured and unstructured activity each day and more on limiting television viewing and media usage.
Of course it, like the other documents, would not be complete without a full presentation of behavior approaches and techniques to use when a child is overweight or obese by BMI along with the drugs of choice and the option for bariatic surgery.
It also justifies the use of a staged behavior modification approach starting with prevention and reaching tertiary care if needed. Unlike the previous documents, it provides more detail by age. Those details make it clear that a child as young as six, when after six-to-twelve months of increasing intensity without sufficient progress, it may then "be appropriate for patient to receive evaluation in tertiary care center," followed by flow-charts to make the decision-making process as to when to step-up intensity a no-brainer.
I really have no problem with the idea of helping parents help their child eat a good diet, I have no problem with encouraging children to be active and play actively each day.
What I do have a problem with is the wholesale implication that children who are overweight and obese are so because they have behaviors which must be modified through intense, staged interventions that have no solid evidence to support their use across the population!
Worsening this is that now, even healthy normal weight children, are to be subject to repeated, routine messages to make it clear they must maintain a BMI within normal or else they too can look forward to intense behavior modification intervention.
You may wonder if anyone has ever investigated how such an approach may affect children long-term?
The last document includes an interesting sentence, "The purpose of this article is to offer practical guidance to providers by providing recommendations, including those that LACK THE BEST POSSIBLE EVIDENCE." (emphasis mine)
It also includes a section titled "Potential Psycological Complications of Behavior-Based Treatment" and states, "Only one study, a 10-year follow-up study of children who completed behavior interventions for obesity, reported on potential complications of treatment. Epstein et al found increased rates of psychiatric disorders such as depression, substance abuse, and eating disorders..." noting it was unclear if these were a result of comorbid conditions associated with obesity.
Amazingly, after staing only one study followed-up on children after behavior intervention, they pooh-pooh this by pointing to another study as supporting behavior intervention comes with little to no risk to children in the future - "Other trials showed improvements in children's psychological functioning and did not find higher rates of eating disorders among children treated with a family-based, behavior, weight management intervention."
I wondered what that study was all about since the clear message here is not to worry about damaging children with this type of intervention. The reference is to a study conducted by Faith et al - Effects of contingent television on physical activity and television viewing in obese children - published in Pediatrics in 2001.
How this expert committee sleeps at night, I don't know!
This is a bait-and-switch citation in what's now being put forth as the standard of care to imply these interventions aren't going to have any long-term consequences to our children's mental health and well-being.
The study referenced, unlike the one that followed up TEN YEARS later, was short-term for twelve weeks, investigating whether making television viewing contingent on a physical activity (pedaling a stationary bike in front of the television) would reduce television viewing time. It did. But it DID NOT investigate any phsycological impacts, nor did it follow up years later to see if there were any psycological impacts.
Nice try though - and anyone reading the document who does not follow the reference trail will never know. Given this type citation madness is included, in what is probably the most important factor - long-term outcome and potential consequences - one must question what else in the document also has this type of reference?
Folks, we have here a plan to now subject every child to intense and routine messages about body weight, BMI, eating, activity and their "behavior" - with no hard evidence it will provide the desired long-term results and the potential to seriously cause harm as our children grow-up in such an environment of intense scrutiny, monitoring and implication that BMI must remain within "normal" or else.
This expert committee has apparently lost all belief in "First Do No Harm."
Tuesday, December 18, 2007
The Perils of Crossing the Establishment Boundaries on Dietary Advice
In the first, Doctor's dietary advice for diabetics not enough, Connie B. Diekman, president of the American Dietetic Association - Chicago, goes to great lengths to reinforce the notion that doctor's are the wrong source of dietary advice and that Registered Dietians are "are more educated about the science of food and nutrition than any other health care professional, but they also know how to translate that science into useful, practical advice that anyone can understand and follow."
She also says that "Dietitians do not simply hand a person a menu. A registered dietitian takes into account a person's age, weight, blood cholesterol levels and other medical needs to develop a plan that is right for that person.
There is no "one-size-fits-all" eating plan for managing diabetes. Patients need to pay attention to portion sizes, timing of meals and specific food choices. They need to eat smart, avoid weight gain and balance the day's food choices with regular physical activity.
A registered dietitian is the best source of advice in all these areas."
In the second, Eat in moderation, the CEO for the American Association of Diabetes Educators - Chicago, Lana Vukovljak, weighs in with - "By touting his "five-fingered diabetic diet" as the key to weight loss and controlled blood glucose, he is perpetuating misinformation and doing his patients a disservice. Eichenbaum advises patients to avoid "bread and baked goods, potatoes and root vegetables, rice, pasta and fruit except for berries." But that diet severely restricts meal plan options, ignores cultural preferences and lifestyle needs, and often results in increased non-compliance. Dietitians and diabetes educators stress the necessity of dietary changes and physical activity. Instead of making broad dietary directives that eliminate entire food groups, however, they encourage moderation and reduced portion sizes. They also make dietary recommendations that factor in an individual's cultural tastes and lifestyle requirements.
Diabetes education helps people incorporate behavior change into their lives by personalizing recommendations and simplifying nutritional messages."
It appears whatever was written by Eichenbaum caused a big stir - two major organizations responded with very clear implications that the author was unqualified and potentially dangerous to patients well-being, thus readers need to ignore whatever it was that appeared in the paper.
What exactly caused the hub-ub?
Well, it was another opinion piece in USA Today, Simple diets work best with diabetes, written by a Dr. Dan Eichenbaum, MD who is an opthamologist in North Carolina.
In that he had the audacity to write, "In numerous studies, elevated blood sugars have been linked to diabetic vision loss despite potentially successful medical and surgical treatments. Medication should be used to control blood sugar only after an optimum diet and exercise regimen has been established.
Most patients, however, expect medication to control blood sugars no matter what they eat. They adjust insulin or pill dosages to cover their dietary indiscretions. Unfortunately, dieticians routinely give patients complex diets that require a ruler, a scale and a calculator. It is no wonder that few diabetics can adhere to these elaborate eating regimens.
I explain to my patients that eating carbohydrates is like putting diesel fuel in a vehicle that can only run on gasoline.
Just as a gas engine won't burn diesel, a diabetic's "engine" cannot burn carbohydrates."
But, he didn't stop there, he also included foods he specifically tells his patients to avoid - bread, pasta, potatoes, baked goods, root vegetables, rice and even fruits except berries. He keeps it simple and says "Patients who eliminate these items lose weight and can easily control their sugar levels. Expecting patients to abide by a diet that is difficult to follow causes non-compliance and increases their risk of blindness."
I point to these today because they highlight the position many clinicians are in when it comes to offering patients dietary advice - they're squarely between a rock and a hard place.
If Dr. Eichenbaum had instead penned something that simply regurgitated the current party-line dietary guidelines, do you think there would have been a similar response questioning his qualifications or patient care?
Hey, have you ever seen Dr. Mehmet Oz slammed in the mainstream media or have his qualifications questioned when he appears on Oprah or Larry King Live espousing the consensus opinion for dietary recommendations?
Of course not - he's preaching the consensus opinion and therefore what he says is okay, his apperances are even highly promoted with viewers encouraged to watch and listen to him. This despite the fact he is not a registered dietitian!
See, as long as your advice is aligned with the consensus, you'll be fine; step outside the boundaries publicly and you'll quickly find your advice ridiculed by the establishment, along with having your qualifications challenged and the clear implication that your patients should wonder if you're harming them!
It does not matter if you've based your advice on hard data from peer-reviewed studies; it certainly doesn't matter that your training as a physician included statistics, biochemistry, biology and other pertinent subjects; and it doesn't matter diddly that your patients see improvements when they follow your advice - what matters is you've crossed the line and made it public that you're dispensing nutrition advice contrary to the current dietary recommendations published by the leading health organizations and you're not a "registered dietitian" to boot.
The above responses to this doctor's words drive home one of our biggest challenges in public healthcare today - the consensus-driven-model that explictly endorses dogma trumping the evidence-based model.
All one needs to do to begin to truly understand how deep this consensus-based-model runs, is to take some time to read through various position statements published by the leading health and medical organizations about what they recommend for diet to clinicians in practice and the public.
Take the American Heart Association position paper on diet, you'll find it's almost identical to that issued by the American Diabetes Association, which is itslef almost identical to that issued by the American Dietetics Association, which is basically the same as the American Cancer Society - the list goes on and on as to this universal message contained within each position statement published by these organizations.
These documents are often held up as the "standards of care" for use in medical practice, informing the clinican that they're written from and based upon the best available evidence, brought together by committee and agreed upon through consensus of those bringing the document together for publication.
These position papers also routinely include references to the alternative approaches that have support in the data, but these are routinely dismissed as inconclusive, deemed controversial, inappropriate or potentially harmful, with the explicit message that no one should advise such an approach to any patient because the evidence is not strong enough. Noticably absent are those studies with the strongest data, while those studies with findings considered minor enough to dismiss are included and highlighted to make the position against their efficacy appear strong.
The interesting thing is, in various position statements, there is a very clear consensus between the organizations when it comes to dietary recommendations - they're all making the same basic recommendations, they all claim to be based on the best available evidence, and they all affirm similar beliefs about macronutrient ratios in a "healthful diet," which leads anyone reading them to believe they're supported by research and evidence from high-quality data. Surely they must be right if all agree on the simple basics!
Wait...wait...wait.....no one seems to ask - are they all so similar because the evidence is so strong and supportive of the dietary recommendations contained within, or are they simply the result of long-held beliefs and dogma driving consensus across organizations?
You can actually begin answer that question yourself.
Simply get your hands on at least three to five position statements from different medical organizations about their dietary recommendations. Then, if you want, you can read them all, but you don't really have to since they're all likely the same bottomline message anyway.
No matter what, your real investigation about the underlying forces driving how the statements are prepared starts in the references.
Look at and compare them in each and between each paper and you'll start to see how they point to each other as basis for supporting evidence and consensus.
It really doesn't matter what organizations you choose - you'll find this "circular reference tactic" within them all, with NONE actually providing conclusive hard data to support their position. They don't need to actually provide mountains of supporting data because with the circular reference tactic, they have each other, and by pointing to the other as supportive and evidence-based they imply the data is "over there" without really doing anything more than taking anyone following the references on a wild goose chase while maintaining the status quo for the the party-line dogma about diet and health.
Then foot soldiers within these organizations will criticize and challenge anyone who dares to not only look beyond these circular reference tactics to find solid evidence that points to an alternative approach, but then actually recommends the alternative to patients and says they do in a public forum, like the media. Such challenges to the status quo simply cannot and will not be tolerated as we can see from the responses above to one doctor who did just that.
Given the strong and dire warnings about the "obesity epidemic" in our country, isn't it time we actually look at the literature and see what the data contains and really hammer out a true evidence-based model of dietary recommendations for the public?
Isn't it time for us to move past this idea "we know" what works, to actually go find out what works based on data and hard evidence?
Friday, December 14, 2007
Glycemic Index Doesn't Matter Much in Overall High-Carb Diet
The short answer - not much when you look for differences between diets that are high or low glycemic index.
But y'all know I'm not about the short answer already, so how about we take a look at a newly published study, No effect of a diet with a reduced glycaemic index on satiety, energy intake and body weight in overweight and obese women, that has some very interesting findings that were notable but ignored in the paper.
Make a note of the paper title, it's important later!
Let's start with some background. For this study, researchers recruited otherwise healthy, obese women who had hyperinsulinemia. They were free of underlying conditions like diabetes, were not taking medications for cholesterol, hypertension or other medical conditions, were not pregnant or breastfeeding, and had not recently dieted to lose weight, nor recently lost or gained weight, thus deemed "weight stable" to participate.
The researchers then determined their habitual food intake and calories consumed each day, noting the subjects consumed an average of 1859-calories/day - 48.8% carbohydrate, 16.7% protein and 34.4% fat [227g carb, 77.6g protein, 71g fat].
The study was then underway, with the women consuming one of two diets for 12-weeks in a cross-over design, so the study lasted a total of 24-weeks. The objective of the study was to "investigate whether a diet with a reduced glycaemic index (GI) has effects on appetite, energy intake, body weight and composition in overweight and obese female subjects," so the researchers provided cereals, breads, rice, pasta and potatoes with different glycemic index for the women to consume while following either the low or the high glycemic diet.
The women were told to consume their foods as they did in their habitual diet and continue eating how they usually ate before starting the study.
In the paper, the researchers noted that "[t]here were no differences in energy intake, body weight or body composition between treatments. On laboratory investigation days, there were no differences in subjective ratings of hunger or fullness, or in energy intake at the snack or lunch meal."
They concluded, "This study provides no evidence to support an effect of a reduced GI diet on satiety, energy intake or body weight in overweight/obese women. Claims that the GI of the diet per se may have specific effects on body weight may therefore be misleading."
Yesterday, Sandy Szwarc at Junkfood Science blog penned her article Carbs humbug? — Are carbs really fattening? about the study, with her perspective being that this is one more piece of evidence that carbohydrates are not fattening.
She wrote, "Despite oft-repeated fears that refined “bad” carbs send our glucose and insulin levels soaring, these researchers found “no differences in glucose, insulin and non-esterfied fatty acid responses to the lower versus higher GI breakfasts, with no differences in either total area under the curve or single measurements at any time point.” Concerns that carbohydrates in the diet stimulate insulin production and are responsible for obesity and illness were recently examined here."
I point to the article at the Junkfood Science blog because it's a good example of seeing the forest while missing the trees.
Let's look at the data in the study now, comparing the dietary changes with their baseline starting values...with the baseline number first, followed by the measured effect of each diet (values are rounded up or down where appropriate).
Low-Glycemic Index Diet, 12-weeks
Baseline - Low-GI Diet
Weight: 87.5kg - 89.1kg
Waist: 103cm - 105cm
Fat Mass: 42.3kg - 44.54kg
Calories: 1859/day - 1928/day
Carbohydrate: 227g/day - 248g/day
Protein: 78g/day - 82g/day
Fat: 71g/day - 69g/day
High-Glycemic Index Diet, 12-weeks
Baseline - High-GI Diet
Weight: 87.5kg - 89.2kg
Waist: 103cm - 106cm
Fat Mass: 42.3kg - 42.9kg
Calories: 1859/day - 1874/day
Carbohydrate: 227g/day - 223g/day
Protein: 78g/day - 83g/day
Fat: 71g/day - 71g/day
The researchers didn't spend much time in the paper discussing the weight gain, fat mass increase, or change in waist circumference. In fact, they noted "[t]here were no differences in body weight, waist circumference or fatness between intervention periods. Weight increased during both intervention periods, although weight gain did not differ between treatments."
They didn't discuss the differences from baseline, nor seek to understand how it is that hyperinsulinemic women, who are obese, gained both weight and body fat while consuming diets that were not that much higher in calories than baseline - certainly not high enough to theoretically gain as much as they did!
But more importantly - look at the increase in waist circumference - more than one inch (3cm) is not something to sneeze at in just 3-months, nor is the scary gain of 4.9-pounds of body fat while consuming the low-GI diet for 12-weeks!
Why did that happen?
The researchers didn't discuss the possibility that high insulin played a role or that blood glucose from carbohydrates consumed had anything to do with it.
Perhaps it happened because insulin and blood glucose didn't budge?
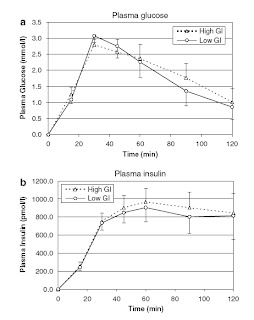
The paper does not include baseline values of insulin and glucose in the table to compare it to each diet, but does provide a telling look at how dietary glycemic index, in the context of a high carbohydrate diet, when compared with each other had no effect on either:
And in case you missed it, what this showed, quite nicely I'll add is that 12-weeks of a high carb diet - whether the perceived junky high-GI or "healthy" low-GI carbs - can make you gain weight, body fat and see your waist grow bigger too...while doing absolutely nothing to resolve a state of hyperinsulinemia!
But yeah, the brilliant conclusion was that there was no difference between low-GI and high-GI...let's not confuse ourselves with the more important findings here!
Monday, December 10, 2007
Low-Carb, Too Much Stress on the Body? Say It Isn't So!
After seeing the article Low carb diets may stress body too much, studies find, on Carol Bardelli's blog, discussion about it on Active Low-Carber Forum, and receiving emails asking me about my thoughts on it, I decided perhaps it's time to add a post here about it.
The article includes one important paragraph that I'll focus on:
The ASU researchers Carol Johnston and Pamela Swan, along with collaborators Sherrie Tjonn and Andrea White, both registered dieticians, and Barry Sears, of the Inflammation Research Foundation and creator of the Zone diet, have published three papers during the last two years, appearing in Osteoporosis International, The American Journal of Clinical Nutrition and most recently in the Journal of the American Dietetic Association.
From the publications above, it's claimed that researchers have found:
1. With these studies, their research uncovered that the ketogenic diet may increase bone loss because of an increase in acid in the body and not enough intake of alkalizing minerals like potassium to neutralize this effect. In addition, a higher percentage of calcium was found in the urine of those on the KLC diet, leading the researchers to believe that the bones are “leaching” calcium.
This would be the finding from the unpublished data included in a Letter to the Editor published in Osteoporosis. It was from a cohort following a low-carb diet or non-ketogenic low-carb diet for two weeks.
Two weeks?
Haven't longer studies reached a different conclusion? The link I just provided is also in the journal Osteoporosis, but it's from a three month study and in it, the researchers concluded, "Although the patients on the low-carbohydrate diet did lose significantly more weight than the controls did, the diet did not increase bone turnover markers compared with controls at any time point. Further, there was no significant change in the bone turnover ratio compared with controls."
2. Another study by these researchers looked at the metabolic advantage of one diet over the other. They found that the reduction in fat loss and weight loss was about the same for both diets over a six-week trial. In addition, body mass index was significantly lower after six weeks in both diet groups. However, those following the KLC diet experienced a greater increase in LDL cholesterol than those following the NLC diet. HDL cholesterol did not seem to be impacted significantly.
This would be from a six week trial comparing the effect of a ketogenic low-carb diet and a non-ketogenic low-carb diet, where the researchers finding was as stated above.
Interesting little problem can be seen, however, when you go to the full-text of the paper - I'm very curious about what they fed (or recommended) those following the ketogenic diet - they managed to get 15g of fiber in them, yet failed to reach recommended intake for folate, vitamin E, iron, magnesium and potassium.
What were they feeding/recommending to these people?
Yes, this is a study I have serious questions about - because it is virtually impossible to miss folate if one is eating non-starchy vegetables as the majority source of carbohydrate, just as it is virtually impossible to miss vitamin E for the same reason. Add to this, failing to meet iron is next to impossible with the combination of meat and leafy greens when one is following a low-carb diet properly, and even magnesium and potassium should come in at levels at least above 80% of recommended intakes.
I even emailed Dr. Sears shortly after the paper was published, asking specifically, "I'm reading through your paper published in the AJCN this month and wondering what was on the menu for both groups? I see the macronutrient and micronutrient values, but am having some difficulty understanding what was provided for meals since some of the nutrient values are quite disparate (like the carbohydrate, cholesterol and polyunsaturated fats). Would it be possible to send me a day's menu of each diet so I can better understand the types of foods the subjects ate during the study?"
Oddly, I received no reply - usually Dr. Sears replies when I email him a question, but with this request for information, he did not. Of course, my request remains open for him or any of his researchers to email me and until such questions are answered about actual food consumed on both diets, the data remains suspect in my opinion since we don't know what was eaten to influence such a nutrient deficiency, which indeed may have influenced the outcomes seen!
3. They also noted that dieters on the NLC diet versus the KLC diet experienced more energy. Their most recent article published in October explains that the body needs carbohydrates for energy so if you are taking in an extremely low amount of carbohydrates and only receiving energy from protein, intense exercise is actually harming your body more than helping it. Without adequate amounts of carbohydrate stores, or glycogen, muscles rapidly fatigue during sustained exercise.
This is from a two-week trial. What's with this two week data offered up as proof these days?
Folks, this one is just a no-brainer. Dr. Steve Phinney has found, and published that time to adapt to a ketogenic diet is required, and once adapted endurance returns to pre-diet levels. That the cohort reported being more fatigued in two weeks is not surprising - in fact, it's expected. "Impaired physical performance is a common but not obligate result of a low carbohydrate diet. Lessons from traditional Inuit culture indicate that time for adaptation, optimized sodium and potassium nutriture, and constraint of protein to 15–25 % of daily energy expenditure allow unimpaired endurance performance despite nutritional ketosis."
Saturday, December 08, 2007
Vegetarian Diet in Pregnancy: Insulin Resistance in Children
The most recent assault on common sense came this week when Newsweek featured The Fertility Diet on its cover, promoting it and the findings from epidemiological data that was the basis of the book as a proven way to eat to enhance fertility. As I noted in my review of the book and study earlier this week, the study findings and book "do not make a proven strategy or evidence-based approach to prevent or reverse ovulatory dysfunction."
I didn't write much about the potential effects on babies born to women consuming such a diet because the post was already very long. However, it needs to be discussed considering new data published this week. For all intents and purposes, The Fertility Diet is recommending a predominently vegetarian diet - limit red meat and animal foods, strictly limit saturated fat, favor protein from beans and include full-fat dairy. This is almost identical to how the population in India eats!
In the abstract we learn the researchers set out to understand how elevated total plasma homocysteine concentrations predict birth weight and risk factors for type II diabetes - "We studied the association between maternal vitamin B12, folate and tHcy status during pregnancy, and offspring adiposity and insulin resistance at 6 years."
To do this they followed 700 pregnant women in six villages (and their children) over six years; "We measured maternal nutritional intake and circulating concentrations of folate, vitamin B12, tHcy and methylmalonic acid (MMA) at 18 and 28 weeks of gestation. These were correlated with offspring anthropometry, body composition (dual-energy X-ray absorptiometry scan) and insulin resistance (homeostatic model assessment of insulin resistance [HOMA-R]) at 6 years."
What the researchers found was not only disturbing, but may have long-term implications not considered critical to long-term health of children previously.
In the table presenting the maternal nutrition data during pregnancy, we learn the women consumed adequate calories - the majority did not consume meat, poultry or fish, but did consume dairy (milk, yougurt, cheese, etc.).
At week 18 of pregnancy, the majority of calories in the diet came from carbohydrate - 70%, fat contributed 17% of energy and protein 13%; at 28 weeks of pregnancy the dietary macronutrient ratios were similar - carbohydrate 72%, fat 16%, protein 12%. The women (without folic acid supplementation) consumed a diet righ with foods high in folate, as evidenced by the finding that only one woman in the whole group was deficient for folate - all others exceeded levels desired in pregnancy.
Alarming however was the finding that the majority were deficient for vitamin B-12 - 60% of the women had blood levels of B-12 less than 150pmol/l. While the finding was alarming, it was not unexpected since the women were not consuming meaningful intakes of animal foods from which we find vitamin B-12 in our diet - the majority of the women were vegetarian, consuming a high carbohydrate, low-fat diet - the type of diet, in fact, promoted in The Fertility Diet book.
The women in the study seem to have done well in their pregnancies and gave birth to healthy babies, some were low birth weight, but as I said, they were overall "healthy."
So why then am I writing about this study?
Well, the effect on their children, over the next six years was telling and speaks volumes about how diet and micronutrient intakes during pregnancy may effect offspring.
When the researchers followed up on the children six years later, they found a seemingly healthy bunch of kids - "At 6 years, the children were light, short and had a low BMI compared with an international (UK) reference; none were overweight or obese as defined by International Obesity Task Force criteria."
You would think that was good news, wouldn't you?
Well, it wasn't their outward appearance or their normal BMI that was problematic, it was their fatness and insulin resistance at age six that shocked the researchers!
"...skinfold thickness measurements showed that the children were relatively truncally adipose; the mean SD score for subscapular skinfold thickness was -0.42 compared with the UK growth standards, in contrast with -2.23 for weight and -1.86 for BMI. Higher fat mass and higher body fat per cent were associated with higher fasting insulin concentrations, higher HOMA-R and higher 120 min plasma glucose concentrations (p = less than 0.05 for all)."
A few paragraphs later we learn, "The highest HOMA-R was in children whose mothers had the lowest vitamin B12 and highest folate concentrations."
What this means is that the children born to women consuming the highest levels of folate rich foods - green leafy vegetables and beans - and the least (or none) animal foods, had children with the highest risk of insulin resistance!
The researchers opened their discussion section bluntly, "We have demonstrated for the first time in a purposeful, community-based prospective study an association between maternal nutritional measurements in pregnancy and two major risk factors for type 2 diabetes in the offspring," and didn't stop there, "higher maternal folate concentrations predicted greater adiposity (fat mass and body fat per cent) and higher insulin resistance, and lower vitamin B12 concentrations predicted higher insulin resistance. Children born to mothers with low vitamin B12 concentrations but high folate concentrations were the most insulin resistant."
They concluded with "...our data raise the important possibility that high folate intakes in vitamin B12-deficient mothers could increase the risk of type 2 diabetes in the offspring. This is the first report in humans to suggest that defects in one-carbon metabolism might be at the heart of intra-uterine programming of adult disease."
If you are pregnant or planning to conceive, you may want to think twice before shunning foods that provide vitamin B-12 - meats, eggs, poultry, fish and dairy!
Friday, December 07, 2007
Free Copy of Protein Power
Here is what Dr. Eades wrote on his blog today:
Through December 20 (after which it will be impossible to get the book by Christmas) we will give away a 1st edition hardcover (not a paperback) copy of the Protein Power LifePlan to anyone of our readers who wants it. That’s right, it’s absolutely free. The price is zero. (Click here to go to the product page on our website and order if you’re interested.)
And in the interest of disclosure, I've got no vested interest here - I saw Dr. Eades post and decided to share the love!
Jonny Bowden Responds to Beverage Association Spin
He recently received an email from the Director of Communications, Tracey Halliday, for the American Beverage Association criticizing his article, saying it was "erroneous" and emphatically stated that "All of our industry's beverages-- including regular or diet soft drinks-- can be part of a healthy way of life when consumed in moderation and as part of a healthy lifestyle."
He responds on his blog.
Enjoy!
With Gene, Carbohydrates Stored as Fat
A high-carb diet has always been considered as a factor behind piling on the pounds. Now, a study in mice conducted by researchers at the University of Wisconsin-Madison has found that the genetic basis as to why this happens. [emphasis mine]
Always? Okay, whatever...
The media is focusing heavily on the supposed "refined" aspect of the carbohydrates consumed by the mice, but abstract itself makes no mention of "refined carbohydrate;" noting the dietary comparison included a high-sucrose, very low-fat diet compared with a high-fat diet to investigate differences in the metabolism of mice with and without the SCD-1 gene.
The lead researcher, James Ntambi, noted, "It looks like the SCD gene in the liver is responsible for causing weight gain in response to a high-carbohydrate diet, because when we take away the gene's activity the animals no longer gain the weight. These findings are telling us that the liver is a key tissue in mediating weight gain induced by excess carbohydrates."
Since this was a study in mice, it was refreshing to see that one article, in the Star, noted that "Human studies have shown that people on high carbohydrate diets have "dramatic" increases in their levels of the SCD enzyme."
While many articles are implying that a drug may be developed to inhibit the gene in humans, Scientific American got to the point quickly, "This finding reveals that the liver determines whether or not eating refined carbohydrates will lead to fat gain. The researchers say this system is a good example of a direct diet-gene interaction. But they also say that a drug to turn off that fat-making liver gene wouldn’t be a good idea. Without that gene, the mice could no longer make glucose. They ended up hypoglycemic—suffering from low blood sugar. So the solution is, sadly, what you already knew: eat fewer processed carbohydrates."
I'd take a step further and say eat fewer carbohydrates, period.
Thursday, December 06, 2007
Housekeeping Update
Thus far, I've managed to maintain the blog ad-free (with the exception of the Amazon Affiliates program linking to books) but have found myself setting aside the blog writing more and more often in favor of other projects...and then missing my blog and the writing and time involved in it!
So, in an effort to see if the blog can cover its own expenses, I'm testing the water with some banner ads. At this point I'm still a bit reluctant and am being very selective about the banner ads I do choose to include here.
For now the advertisements you see, I can assure you that they meet certain conditions if they're here:
1. I have purchased product or service from the company and was very satisfied with service, product and customer care
2. No companies have a "dog in the fight" of diet and nutrition
3. Some have something "valuable" to offer - like uPromise for college savings (I've been a member myself since before my son was born)
4. As always, if it's a book, I've purchased it myself, read it and recommend it (expcet where noted - ie. Gary Taubes, Good Calories, Bad Calories)
I'll evaluate how things are going with this in 90-days and consider reader comments and feedback about whether to continue after the 90-days pass. I'll be mixing things up - adding banners at the end of posts, in the sidebar, and in the footers.
Thank you for your patience!
What's Inside?
I wish the video didn't freeze on the frame that gives away the end, but it's still worth the view!
Wednesday, December 05, 2007
Must See Videos
PART 1: Cholesterol
PART 2: Familial Hypercholesterolemia
PART 3: Statins
PART 4: Heart Disease
PART 5: CVD Populations
If you like the video presentation given by Dr. Malcolm Kendrick, you may want to read his book,The Great Cholesterol Con: The Truth About What Really Causes Heart Disease and How to Avoid It
Real Food Versus Enriched Flour
This is what happens when one believes the best source of folic acid is enriched white flour, an ingredient universally shunned by those following a low carbohydrate diet. It's important to note that folic acid is the synthetic form of folate which is found naturally in vegetables, citrus fruits, legumes and even liver.
So why the worry about a low carbohydrate diet?
It seems the powers that be fail to appreciate just how easy it is to meet and exceed folate recommendations with food alone. Rather than express real concern over the poor dietary habits in the United States, they'll push for more fortification of the nutritionally bankrupt food being consumed.
The current recommendation for folic acid/folate is 400mcg a day. Want to see just how easy it is to meet that intake with real food?
A salad made with 2-cups shredded romaine, 1/4 cup shredded red cabbage, 4 cherry tomatoes and 1/3 of a medium cucumber along with 1-cup cooked spinach provides 437.5mcg of folate before any other folate containing foods are included in the day.
That is what someone following a low carbohydrate diet might choose to eat in a day since it provides just 84-calories, 15g total carbohydrate and 8g of fiber, providng just 7g net carbohydrate in their day.
Once they add in other options to their day their intake of folate will rise, although how much they consume at the end of the day will depend upon their choices.
But one thing is clear here - with a salad and a cup of spinach, they've met and exceeded the recommended intake!
I've said it many times - eat real food, eat good food and eat foods rich with nutrients. In this case, eating your non-starchy vegetables is a great way to meet and exceed requriements for folate!
Tuesday, December 04, 2007
Don't Buy Their Snake Oil
But, they didn't simply publish a paper. No, they also published a book - The Fertility Diet - that is now featured on the cover of Newsweek and also being touted in the media as the low-tech, do-it-yourself way to prevent and even reverse ovulatory infertility!
Worse though is the media advancing the findings in a way that implies the dietary strategy has been tested in infertile women!
Take a look at how MedScape opened their article - "Higher intake of monounsaturated fats; vegetable protein; and high-fiber, low-glycemic carbohydrates improved fertility outcomes in women with ovulatory disorder infertility, according to the results of a cohort study reported in the November issue of Obstetrics & Gynecology."
The data is not from women who specifically had a diagnosis of ovulatory dysfunction (irregular or absent menstruation). Rather, the data was from a cohort of women within the Nurse's Health Study II who were identified as actively trying to get pregnant during the period of follow-up data collection. That is a very different cohort of subjects than one exclusively made up of women with infertility, or a cohort designed as a comparison study of women with and without fertility issues due to ovulation!
But the thing that really irks me is the media falling all over itself to highlight one finding in particular, the supposed reduction of ovulatory dysfunction if women follow the dietary strategy outlined in the book - "their research shows that women who follow five or more of the tips could boost their fertility by up to 80 percent," is how the Boston Channel presented it.
Charles Platkin (Diet Detective) wrote, "In fact, the Nurses’ Health study showed that those who did not follow a healthy diet were six times more likely to experience infertility related to ovulation than women who did."
Oh really?
How about we look at the published data - let's look specifically at those cases with ovulatory disorder infertility published in the study:
Diet Score .Cases .RR (95% CI)
Q1 (lowest) _117 _1.00
Q2 _100 _0.68 (0.52 - 0.89)
Q3 _77 _0.65 (0.48 - 0.87)
Q4 _80 _0.53 (0.40 - 0.72)
Q5 _42 _0.34 (0.23 - 0.48)
Do you see a six-fold difference between Q1 and Q5? I didn't think so!
Do you see an 80% greater chance of pregnancy in those in Q5 than those in Q1? I didn't think so!
And as an aside - I don't get is how in Q4 they reported more cases of infertility, yet managed to report a lower RR? Anyone want to help me out with that one?
Anyway, I was scratching my head, trying to figure out how they came up with these incredible numbers - statistics being used to heavily promote the book right now - and they're in the study all right, in a theoretical computer model (which should be called a fantasy search for significance) run with different scenarios of possibilities, not data of real women eating in the real world!
As the researchers noted in their paper, "we calculated the population attributable risk associated with specific combinations of dietary and lifestyle factors to estimate the proportion of cases that may have been avoided had all the women in this cohort adhered to these habits."
So now, rather than state these numbers are based on computer models and are, at best, theoretical - they're promoting the book as if it's fact that the dietary strategies actually work.
And they're doing it in a way that is promoting the idea that a woman with ovulatory dysfunction can fix it herself, without medical intervention, and get pregnant on her own.
To say this is a travesty for women's health is an understatement!
Just when you think it's not possible, it really does get worse.
If the promotion of theoretical as fact isn't bad enough, here is a real hard fact that should send chills up your spine - while the majority of cases of ovulatory dysfunction are attributed to PCOS (polycystic ovarian syndrome), a large enough number are due to hyperprolactenemia, usually cased by a small tumor at the base of the brain. Yet, the book has absolutely no warning to women that a diagnosis for the cause of ovulatory dysfunction is critical before beginning the do-it-yourself diet approach.
Think about that for a moment.
Then consider that ovulatory dysfunction can also be due to disease of the pituitary, adrenal or thyroid glands. It can also be due to premature ovarian failure (premature menopause).
Without a diagnosis, you're flying blind as to cause and without any warning in the book about the many causes of ovulatory dysfunction, you may in fact be delaying critical medical intervention to resolve the problem if you simply take the book and run with the recommendations.
Oh and it just keeps going too. Also noticeably absent is any warning to women already experiencing ovulatory dysfunction that continuing to attempt pregnancy in the absence of regular menstruation is futile. In fact the book promotes the standard advice that one year of trying to get pregnant is recommended unless one is over 35, then six months of trying is appropriate before seeking a medical evaluation.
When a woman has a regular cycle, this advice is fine - when she has absent or irregular periods, she's wasting precious time continuing along and trying without a diagnosis because without ovulation there cannot be a pregnancy!
One recommendation in particular can also be problematic for a woman already experiencing ovulatory dysfunction - the recommendation to increase iron intake. You see, if the researchers who wrote the book bothered to look at the literature, they'd have learned that women with ovulatory dysfunction often have elevated stores of iron. As the researchers in the above linked study noted, "Because the periodic blood loss resulting from regular menstruation protects pre-menopausal women against excessive iron accumulation, oligomenorrhea and amenorrhea might contribute to the increase in ferritin observed in overweight and obese PCOS patients. When studying PCOS patients and control subjects as a whole, ferritin levels were increased in women with amenorrhea compared with women with regular menstrual cycles, whereas women with oligomenorrhea presented with intermediate values (means ± SD: amenorrhea 159 ± 144 pmol/l, oligomenorrhea 114 ± 95 pmol/l, and regular menstrual cycles 83 ± 51 pmol/l; F = 3.295, P = 0.040)."
Also of note is the fact that in the book they recommend reducing saturated fat intake to less than 8% of calories.
Where, pray tell, is the data to support that recommendation?
It certainly isn't in their published paper. In their published data, the women with the lowest risk of infertility not only consumed the highest level of total fat, but their intake of saturated fat was also higher than the other groups - in fact, their saturated fat intake accounted for 11.5% of calories.
But hey, let's not let the actual data get in the way of recommendations that align with the author's previous book, Eat, Drink and Be Healthy!
While we're at it, where is the data to support eating less meat? Their published data found absolutely no difference in heme iron intake between the various groups - none at all - yet they're promoting the idea that reducing red meat in the diet is going to make a difference in getting pregnant. Their data does not support this idea; and add to that this idea has not even been tested in women attempting to get pregnant, yet that doesn't stop them from making the recommendation.
Worse though (can it really get worse?) is the inclusion within the book of the politically correct idea that reducing or even eliminating red meat is better for the environment - who needs data when you can convince women to limit or eliminate red meat on emotion.
If you're a woman wanting to get pregnant, do you want to based your diet on politically correct advice or hard evidence?
Do you want to make changes to your diet based on theoretical computer models, or data from studies that have actually investigated how a change to diet improved pregnancy rates in those participating in the study?
As Albert Einstein once pointed out, "Only two things are infinite, the universe and human stupidity, and I’m not sure about the former."
Stupidity or just plain old ignorance contributes greatly to the millions of people who succumb daily to the latest or most heavily promoted "facts" generated by epidemiologist's findings concerning diet. Today it happens to be diet and fertility, tomorrow it'll be diet and aging, the next day diet and cancer.
The problem though, with such data from epidemiological studies on diet and lifestyle, remains (and will forever remain) that correlation does not imply causation. I don't know how many times that can be repeated, but it is true and will always be true. Just as it is true that eating red meat does not cause ovulatory dysfunction anymore than consuming high levels of non-heme iron prevents it. Just as consuming regular ice cream does not make you fertile anymore than restricting saturated fat to less than 8% of your calories will make you get pregnant.
That the media is heavily promoting this book only tells us one thing - they don't understand science, the scientific method, or the difference between correlation and causation. And they certainly have not read the study in full and then compared it to the book's recommendations.
No doubt the findings are intriguing, but they do not make a proven strategy or evidence-based approach to prevent or reverse ovulatory dysfunction.
What they do provide is a starting point to actually test the dietary strategies in women with ovulatory dysfunction. Until those studies are conducted, the book is merely speculation, potentially a waste of precious time or worse for a woman with ovulatory dysfunction.
On this book I have to strongly suggest taking a pass and instead do what's best - go to the doctor if you're having problems getting pregnant or have irregular or absent periods. Without a diagnosis, you're flying blind on assumptions - it's better to have a diagnosis and tackle the problem based on facts rather than guessing what's wrong. It's true that you can make changes in your diet and see improvement, just as it's true that if your ovulatory dysfunction is caused by a tumor your diet isn't going to make a difference.
Just because the book is from esteemed researchers at Harvard doesn't mean it isn't snake oil.
Monday, December 03, 2007
You are what your body does with what you eat
The press release, issued from SUNY Downstate, sums it up completely:
Metabolic syndrome is a condition afflicting one quarter to one third of adult men and women and is an established pre-cursor to diabetes, coronary heart disease, and other serious illnesses. Patients have long been advised to eat a low-fat diet even though carbohydrate restriction has been found to be more effective at reducing specific markers, such as high triglycerides, characteristic of the syndrome. Now, a new study indicates that a diet low in carbohydrates is also more effective than a diet low in fat in reducing saturated fatty acids in the blood and reducing markers of inflammation.
While there have been contradictory and confusing messages directed at health conscious consumers about dietary recommendations, most researchers agree on the need to limit inflammatory agents. In a report published today in the on-line version of the journal Lipids, researchers at the University of Connecticut, SUNY Downstate Medical Center in Brooklyn, and the University of Minnesota show much greater improvement in inflammatory markers in patients with metabolic syndrome on a very low carbohydrate approach compared to a low fat diet.
Lead researcher Jeff S. Volek, PhD, RD, associate professor of kinesiology at the University of Connecticut, describes the study as “adding to the evolving picture of improvement in general health beyond simple weight loss in keeping blood glucose and insulin under control.” The work is part of a larger study (currently under review) showing numerous improvements in blood lipids.
The current work concludes that “lowering total and saturated fat only had a small effect on circulating inflammatory markers whereas reducing carbohydrate led to considerably greater reductions in a number of pro-inflammatory cytokines, chemokines, and adhesion molecules. These data implicate dietary carbohydrate rather than fat as a more significant nutritional factor contributing to inflammatory processes.”
Richard Feinman, PhD, professor of biochemistry at SUNY Downstate Medical Center, adds, “The real importance of diets that lower carbohydrate content is that they are grounded in mechanism: carbohydrates stimulate insulin secretion which biases fat metabolism towards storage rather than oxidation. The inflammation results open a new aspect of the problem. From a practical standpoint, continued demonstrations that carbohydrate restriction is more beneficial than low fat could be good news to those wishing to forestall or manage the diseases associated with metabolic syndrome.”
One of the remarkable effects in the data presented that may have contributed to the results is that despite the three-fold greater saturated fat in the diet for the low carb group, saturated fat in the blood turned out to be higher in the low fat group due to the process known as carbohydrate-induced lipogenesis.
Dr. Volek points out that “this clearly shows the limitations of the idea that ‘you are what you eat.’ Metabolism plays a big role. You are what your body does with what you eat.”






